International Journal of Periodontics & Restorative Dentistry, Pre-Print
DOI: 10.11607/prd.7290, PubMed-ID: 392412206. Sept. 2024,Seiten: 1-30, Sprache: EnglischAroca, Sofia / Zucchelli, Giovanni / Di Domenico, Giovanna Laura / de Sanctis, MassimoThe multiple coronally advanced flap (MCAF) and the modified coronally advanced tunnel technique (MCAT) are the most commonly used methods for treating multiple gingival recessions. However, treating multiple defects is very complex due to various biological and anatomical factors, and there is no clear guideline on the major or minor determinants that influence surgical decisions. The aim of the present commentary is to discuss a decision tree to suggest to clinicians the most relevant anatomical factors to take in to consideration when evaluating the choice between a MCAT and an MCAF. In the proposed decision-making process, the first crucial step involves the evaluation of the interdental clinical attachment loss (CAL), according to the new EFP/AAP classification. The next step is to assess the dimensions of the lateral keratinized tissue (LKT), that is the keratinized tissue located laterally to the recession defect. When LKT amount is insufficient, the size of the interdental papillae, including base, height, and coronal width, must also be evaluated.
Schlagwörter: mucogingival surgery, gingival recession, decision tree, connective tissue graft
International Journal of Periodontics & Restorative Dentistry, Pre-Print
DOI: 10.11607/prd.7346, PubMed-ID: 3945362225. Okt. 2024,Seiten: 1-20, Sprache: EnglischZucchelli, Giovanni / Mounssif, Ilham / Mazzotti, Claudio / Bentivogli, Valentina / Rendon, Alexandra / Sangiorgi, Matteo / Stefanini, MartinaImpairment or loss of interdental papilla is a common issue in patients with periodontal disease, leading to phonetic, functional, and aesthetic concerns. Numerous techniques have been explored to reconstruct and regenerate interdental papillae, but consistent success remains challenging. This article presents a novel surgical approach that applies the principles of the Connective Tissue Graft (CTG) wall technique to enhance papilla volume when interdental clinical attachment loss is present in the aesthetic zone. The case of a 35-year-old woman with an RT3 recession defect associated with loss of interdental hard and soft tissues is discussed. The patient underwent a procedure involving palatal incisions, application of amelogenins, and a trapezoidal shape CTG fixed at the base of the papilla under a coronally advanced flap. This approach aimed to stabilize the blood clot and prevent soft tissue collapse into the defect area, enhancing the position and volume of the interdental papilla. Results at 6- and 12-months follow-up indicated significant improvement in papilla appearance and complete root coverage. This case suggests that the modified CTG wall technique can effectively treat buccal and interdental gingival recessions associated with horizontal or infrabony defects. Further clinical trials are necessary to confirm these findings and establish the most effective approach for interdental papilla reconstruction.
Schlagwörter: interdental papilla, connetive tissue graft, periodontal therapy, amelogenins, connective tissue graft-wall technique, papilla reconstruction
International Journal of Periodontics & Restorative Dentistry, Pre-Print
DOI: 10.11607/prd.7286, PubMed-ID: 392703116. Sept. 2024,Seiten: 1-24, Sprache: EnglischPalombo, David / Mascetti, Tommaso / Zucchelli, Giovanni / Sanz, MarianoThe management of severe mucogingival deformities surrounding malpositioned implants represents a complex issue with a high risk of aesthetic failure. The present case report describes a mucogingival and restorative approach for the treatment of severe localized peri-implant tissue deficiencies with interproximal bone loss combined with an interproximal gingival recession on the adjacent natural tooth. This consists of maintaining a non-restorable malpositioned implant, submerging it through one or multiple vertical soft tissue augmentations, according to the defect severity, and delivering a tooth supported bridge involving the adjacent natural teeth. The step-by-step surgical technique adopted for implant submergence and vertical soft tissue grafting, as well as the subsequent surgical and prosthetic interventions, are described, presenting results at 5 years from implant submergence and 3 years from prosthetic finalization.
Schlagwörter: Implants, Periodontal Surgery, Prosthetic Dentistry, Gingival Recession, Mucogingival Surgery, Dental Implant, Case Report
International Journal of Periodontics & Restorative Dentistry, Pre-Print
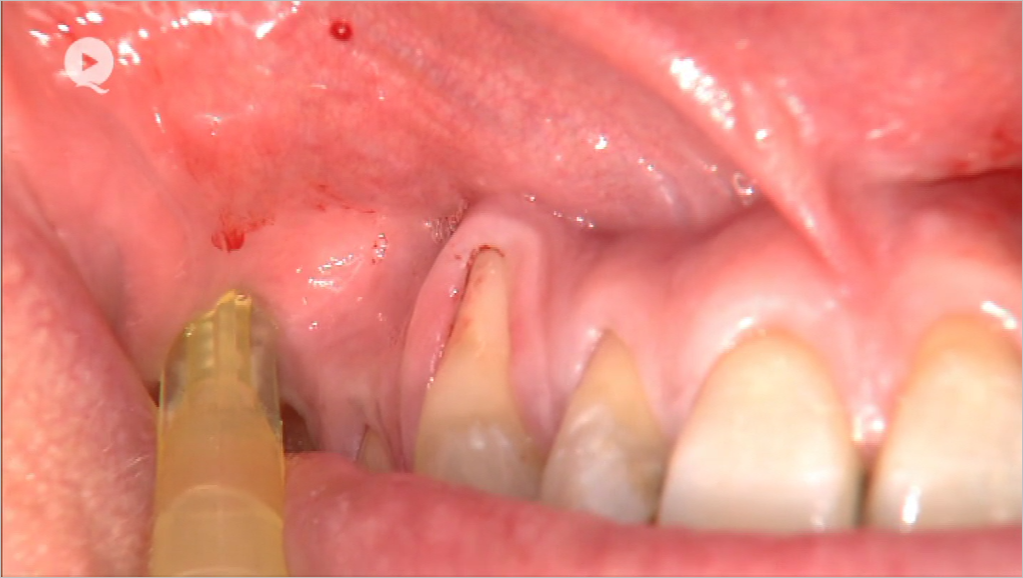
DOI: 10.11607/prd.7600, PubMed-ID: 401987758. Apr. 2025,Seiten: 1-16, Sprache: EnglischDe Stavola, Luca / Zucchelli, GiovanniThe soft tissue management in bone augmentation is critical to ensure the predictability of new bone formation. The flap elongation, by periosteum releasing incision, determines an anatomical alteration of the existing soft tissue architecture. In particular the vestibule position as well as the muco-gingival line are moved coronally. The correction of the vestibule position is usually performed by a partial flap preparation very closed to the periosteum layer reducing the overall supra-crestal tissue volume. The presented technique defines the strategy to obtain a flap elongation potentially without the loss of the vestibule position. Clear anatomical reference points are introduced and described to render the technique replaceable and predictable.
International Journal of Esthetic Dentistry (DE), 2/2024
Clinical ResearchSeiten: 124-136, Sprache: DeutschGalli, Fabio / Deflorian, Matteo / Zucchelli, Giovanni / Del Fabbro, Massimo / Testori, TizianoEine retrospektive Studie mit 5 bis 13 Jahren NachbeobachtungZiel: In der vorliegenden retrospektiven Studie sollten die klinischen Ergebnisse von festsitzendem, auf den Prinzipien der biologisch orientierten Präparationstechnik (BOPT) basierenden Zahnersatz über mittlere bis lange Beobachtungszeiträume ausgewertet werden.
Material und Methoden: Die Behandlungsdokumentation von Patienten, die zwischen Januar 2007 und Dezember 2014 festsitzend rehabilitiert worden waren, wurden retrospektiv ausgewertet. Patienten, deren Akten die Einschlusskriterien erfüllten, wurden außerdem zu einer abschließenden Kontrolluntersuchung einbestellt. Ausgewertet wurden die parodontalen Parameter, das Vorliegen von Gingivarezessionen sowie die aufgetretenen technischen und biologischen Komplikationen.
Ergebnisse: Insgesamt 58 Patienten wurden per Recall eingeladen. Von diesen konnten 52 Patienten mit 220 überkronten Zähnen ausgewertet werden (Ausfallrate: 13,8 %). Die durchschnittliche Beobachtungsdauer waren 9,3 Jahre (Spannweite 5 bis 13 Jahre): 14 Patienten (114 überkronte Zähne) waren 5 bis 8 Jahre, 36 Patienten (106 überkronte Zähne) 9 bis 13 Jahre nachbeobachtet worden. Die prothetische Überlebensrate betrug 99,6 %. An Komplikationen waren eine Wurzelfraktur (0,4 %) und vier Verblendkeramikabplatzungen (1,8 %) dokumentiert. Sechs Zähne (2,7 % der untersuchten Kronen) zeigten eine Gingivarezession von < 1 mm und 13 Zähne (24 Stellen) wiesen eine Sondierungstiefe von 4 mm auf (5,9 % der prothetischen Kronen/1,8 % der sondierten Stellen). Schließlich wurde an 20 Stellen (1,5 %) bzw. 7 Zähnen (3,2 %) Sondierungsbluten beobachtet.
Schlussfolgerungen: Die Präparation nach den BOPT-Regeln (d. h. mit vertikaler, kantenfreier Präparation) führte mittel- bis langfristig zu einem gesunden Parodont und stabiler Gingiva. Das prothetische Behandlungsergebnis blieb dauerhaft erhalten.
Schlagwörter: biologisch orientierte Präparationstechnik, BOPT, parodontale Gesundheit, Gingivarezession, Weichgewebestabilität, retrospektive Studie
International Journal of Esthetic Dentistry (EN), 2/2024
Clinical ResearchPubMed-ID: 38726854Seiten: 112-124, Sprache: EnglischGalli, Fabio / Deflorian, Matteo / Zucchelli, Giovanni / Del Fabbro, Massimo / Testori, TizianoA 5- to 13-year follow-up retrospective studyAim: The present study was a retrospective medium- to long-term follow-up assessment of the clinical outcomes of patients rehabilitated with fixed prostheses according to the biologically oriented preparation technique (BOPT) principles.
Materials and methods: Clinical records of patients rehabilitated between January 2007 and December 2014 were retrospectively assessed. Patients whose records met the inclusion criteria were also recalled for a hygiene visit. Data analyzed included the patients’ periodontal condition, the presence of gingival recessions as well as any technical or biologic prosthetic complication.
Results: Fifty-eight patients were recalled; of these, 52 patients who had received 220 crowns were available for the evaluation (the dropout being 13.8%). The average follow-up was 9.3 years (range 5 to 13 years): 14 patients (114 prosthetic crowns) had a follow-up between 5 and 8 years, and 36 patients (106 prosthetic crowns) between 9 and 13 years. The prosthetic survival rate was 99.6%. One radicular fracture (0.4%) and four chippings of the veneering porcelain (1.8%) were recorded. Six teeth (2.7% of the examined prosthetic crowns) presented gingival recession of < 1 mm, and 13 teeth (24 sites) had a pocket probing depth of 4 mm (5.9% of the prosthetic crowns/1.8% of the sites). Finally, 20 sites (1.5%) in seven teeth (3.2%) showed bleeding on probing.
Conclusions: Tooth preparation according to the BOPT principles (ie, with a vertical finishing line) resulted in medium- to long-term periodontal health and stability of the gingival tissue, and prosthetic success was maintained.
Schlagwörter: BOPT, periodontal health, gingival recession, soft tissue stability, retrospective study
International Journal of Oral Implantology, 1/2024
PubMed-ID: 38501401Seiten: 89-100, Sprache: EnglischTestori, Tiziano / Clauser, Tommaso / Rapani, Antonio / Artzi, Zvi / Avila-Ortiz, Gustavo / Barootchi, Shayan / Bressan, Eriberto / Chiapasco, Matteo / Cordaro, Luca / Decker, Ann / De Stavola, Luca / Di Stefano, Danilo Alessio / Felice, Pietro / Fontana, Filippo / Grusovin, Maria Gabriella / Jensen, Ole T / Le, Bach T / Lombardi, Teresa / Misch, Craig / Pikos, Michael / Pistilli, Roberto / Ronda, Marco / Saleh, Muhammad H / Schwartz-Arad, Devorah / Simion, Massimo / Taschieri, Silvio / Toffler, Michael / Tozum, Tolga F / Valentini, Pascal / Vinci, Raffaele / Wallace, Stephen S / Wang, Hom-Lay / Wen, Shih Cheng / Yin, Shi / Zucchelli, Giovanni / Zuffetti, Francesco / Stacchi, ClaudioPurpose: To establish consensus-driven guidelines that could support the clinical decision-making process for implant-supported rehabilitation of the posterior atrophic maxilla and ultimately improve long-term treatment outcomes and patient satisfaction.
Materials and methods: A total of 33 participants were enrolled (18 active members of the Italian Academy of Osseointegration and 15 international experts). Based on the available evidence, the development group discussed and proposed an initial list of 20 statements, which were later evalu-ated by all participants. After the forms were completed, the responses were sent for blinded ana-lysis. In most cases, when a consensus was not reached, the statements were rephrased and sent to the participants for another round of evaluation. Three rounds were planned.
Results: After the first round of voting, participants came close to reaching a consensus on six statements, but no consensus was achieved for the other fourteen. Following this, nineteen statements were rephrased and sent to participants again for the second round of voting, after which a consensus was reached for six statements and almost reached for three statements, but no consensus was achieved for the other ten. All 13 statements upon which no consensus was reached were rephrased and included in the third round. After this round, a consensus was achieved for an additional nine statements and almost achieved for three statements, but no consensus was reached for the remaining statement.
Conclusion: This Delphi consensus highlights the importance of accurate preoperative planning, taking into consideration the maxillomandibular relationship to meet the functional and aesthetic requirements of the final restoration. Emphasis is placed on the role played by the sinus bony walls and floor in providing essential elements for bone formation, and on evaluation of bucco-palatal sinus width for choosing between lateral and transcrestal sinus floor elevation. Tilted and trans-sinus implants are considered viable options, whereas caution is advised when placing pterygoid implants. Zygomatic implants are seen as a potential option in specific cases, such as for completely edentulous elderly or oncological patients, for whom conventional alternatives are unsuitable.
Schlagwörter: diagnostic procedure, implant dentistry, lateral window technique, pterygoid implants, sinus floor elevation, transcrestal sinus floor elevation, zygomatic implants
The authors report no conflicts of interest relating to this study.
International Journal of Periodontics & Restorative Dentistry, 3/2023
DOI: 10.11607/prd.6538, PubMed-ID: 37141083Seiten: 281-288, Sprache: EnglischTavelli, Lorenzo / Heck, Teresa / De Souza, André B / Stefanini, Martina / Zucchelli, Giovanni / Barootchi, ShayanImplant esthetic complications can negatively affect a patient's perception of implant therapy and their quality of life. This article discusses the etiology, prevalence, and strategies for the treatment of peri-implant soft tissue dehiscences/deficiencies (PSTDs). Three common scenarios of implant esthetic complications were identified and described, in which PSTDs could be managed without removing the crown (scenario I), with the surgical-prosthetic approach (crown removal; scenario II), and/or with the horizontal and vertical soft tissue augmentation and submerged healing (scenario III).
International Journal of Esthetic Dentistry (DE), 2/2023
The Last PageSeiten: 218, Sprache: DeutschZucchelli, GiovanniThe International Journal of Prosthodontics, 2/2023
DOI: 10.11607/ijp.7591, PubMed-ID: 36445219Seiten: 228-232, Sprache: EnglischMonaco, Carlo / Scheda, Lorenzo / Arena, Antonio / di Fiore, Adolfo / Zucchelli, GiovanniPurpose: To describe the treatment of malpositioned implants in the esthetic area using the angulated welded abutment (AWA) approach together with peri-implant soft tissue surgery.
Materials and Methods: A clinical case with extreme buccal angulation of two implants in the anterior maxilla was used to illustrate the AWA technique. After implant impression-taking, digital analysis was used to determine the ideal prosthetic angulation of the abutment and the ideal position of its screw hole in relation to the gingival margin of the adjacent teeth. The AWA was designed in two combinable components that were meant to be welded together. Before the welding process, an angulated screw was included in the abutment. Since the angulated screw was inside the abutment, the screwdriver hole could be designed as narrow as possible and put in an ideal position. After periodontal and peri-implant surgery were carried out, the AWA was applied to the implants.
Results: The AWA allowed correction of the prosthetic axis. Moreover, relocation of the screw hole allowed the gingival tissue to creep over the abutment. In this way, a new esthetic restoration can be placed after the mucogingival surgery.
Conclusion: The excessive misangulation of the implants was efficiently recovered. Further studies are needed to evaluate long-term clinical success, and standardization of this technique is required for routine clinical use.