Oral Health and Preventive Dentistry, 1/2021
Open Access Online OnlyRandomised Controlled Clinical TrialDOI: 10.3290/j.ohpd.b966767, PubMed-ID: 3361576919. Feb. 2021,Seiten: 137-147, Sprache: EnglischA. Ramseier, Christoph / Petitat, Chloé / Trepp, Sidonia / Lang, Niklaus P. / Eick, Sigrun / Adam, Ralf / Ccahuana-Vasquez, Renzo A. / Barker, Matthew L. / Timm, Hans / Klukowska, Malgorzata / Salvi, Giovanni E.Purpose: To compare clinical outcomes and oral fluid biomarkers in gingivitis subjects using an electric toothbrush/irrigator combination (test) or a manual toothbrush alone (control) over 8 weeks.
Materials and Methods: Subjects were randomly assigned to two groups of n = 30. In both groups, toothbrushing was performed twice daily at home and no additional interdental cleaning aids were allowed. Plaque Index (PLI), Gingival Index (GI), whole saliva (WS), and gingival crevicular fluid (GCF) samples were collected at weeks 2, 4, and 8.
Results: Subjects’ mean age was 23 years and 52% were female. Overall baseline means were 1.31 for PLI, 1.07 for GI, and 34.9 for number of bleeding sites. At every follow-up visit, both groups differed statistically significantly (p < 0.001) from baseline for all clinical parameters. The test group demonstrated statistically significantly (p < 0.001) greater reductions in GI vs the control group by 18% at week 2, 17% at week 4 and 24% at week 8. The test group also demonstrated statistically significantly (p < 0.002) greater reductions in the number of bleeding sites vs the control group by 33% at week 2, 34% at week 4 and 43% at week 8. Between-group comparisons for both WS and GCF revealed numerical trends for decreased levels of interleukin (IL)-1β in GCF after 4 and 8 weeks, but these were not statistically significant.
Conclusion: In subjects using the electric toothbrush/irrigator combination, increased clinical improvements may be found accompanied by similarly improved trends for oral fluid biomarkers such as IL-1β.
Schlagwörter: gingival crevicular fluid, gingivitis, prevention, toothbrushing
Implantologie, 2/2020
Seiten: 117-127, Sprache: DeutschDe Ry, Siro P. L. / Roccuzzo, Andrea / Sculean, Anton / Salvi, Giovanni E.Periimplantäre Erkrankungen sind entzündliche Reaktionen der periimplantären Gewebe auf bakterielle Kontamination an osseointegrierten Implantaten. In den vergangenen Jahren hat das wissenschaftliche Interesse an diesem Thema zugenommen, wie die große Zahl der vorgeschlagenen Protokolle zur Behandlung der periimplantären Mukositis und der Periimplantitis zeigt. Ziel der vorliegenden Übersichtsarbeit ist es, einen Überblick über die in den letzten 5 Jahren veröffentlichten Protokolle für die nichtchirurgische Behandlung periimplantärer Erkrankungen zu geben. Hierbei wurden auch neueste adjuvante und alternative Maßnahmen zur mechanischen Reinigung berücksichtigt und untersucht, die eingesetzt werden, um eine Dekontamination der Implantatoberfläche und Beseitigung von Entzündungen der periimplantären Gewebe zu erzielen. Jedoch konnte keine der adjuvanten Maßnahmen eine statistisch signifikante Verbesserung der periimplantären Verhältnisse im Vergleich zur alleinigen nichtchirurgischen mechanischen Reinigung zeigen. Zusammengefasst haben sich nichtchirurgische Konzepte für die Behandlung periimplantärer Erkrankungen als zuverlässig erwiesen, wenn es darum geht, klinische Anzeichen periimplantärer Entzündungen zu reduzieren, auch wenn sie nur begrenzt in der Lage sind, eine vollständige Heilung der Krankheit zu erzielen. Die Anwendung adjuvanter Mittel, wie Chlorhexidin, Lasern, fotodynamische Therapie, systemische Probiotika, sollte weiter erforscht werden, da ein Nutzen bislang nicht oder nur begrenzt gezeigt werden konnte.
Schlagwörter: Titan, Zahnimplantate, periimplantäre Erkrankungen, periimplantäre Mukositis, Periimplantitis, Entzündungen, krestaler Knochenverlust
Quintessence International, 1/2020
DOI: 10.3290/j.qi.a43048, PubMed-ID: 31463483Seiten: 28-36, Sprache: EnglischIorio-Siciliano, Vincenzo / Blasi, Andrea / Sammartino, Gilberto / Salvi, Giovanni E. / Sculean, AntonObjectives: To assess the stability of soft tissues around implants by comparing mucosal recessions in patients with keratinized mucosa (test) with patients without keratinized mucosa (control) around osseointegrated dental implants.
Method and materials: The PICO criteria used were as follows: Population, patients with osseointegrated dental implants; Intervention/exposure, presence of a keratinized mucosa; Comparison/control, absence of keratinized mucosa; Outcome, presence or absence of peri-implant mucosal recessions (mm).
Data sources: An electronic search of Medline, Embase, and Cochrane Oral Health Group specialist trials supplemented by manual searching was conducted to identify studies reporting outcomes of at least 5 years on the presence of mucosal recessions at implants with or without attached mucosa. Mucosal recession (MR) was set as primary outcome. Prospective cohort studies published in English language up to October 2018, with a mean follow-up period of at least 5 years, reporting keratinized tissue height ≥ 2 mm and 2 mm or presence/absence of keratinized tissue, with fixed implant-supported prostheses. The homogeneity of studies was assessed by DerSimonian and Laird test (Q test). The differences in terms of gingival recession around implants reported between test groups (keratinized mucosa ≥ 2 mm) and control (keratinized mucosa 2 mm or no keratinized mucosa) were compared. Two studies reporting 201 patients with 514 tissue level implants were selected for the final analysis.
Results: Due to the high heterogeneity between the selected studies, no statistical test could be performed. However, in both studies a deeper mucosal recession occurred when keratinized mucosa was 2 mm: 0.61 ± 0.10 (−0.90; −0.32) and −1.92 ± 0.12 (−2.16; −1.68), respectively.
Conclusion: Within their limitations, the findings indicate that after a mean observation period of at least 5 years, the presence of keratinized mucosa may lead to less mucosal recession at dental implants.
Schlagwörter: dental implants, keratinized mucosa, mucosal recession, systematic review
Oral Health and Preventive Dentistry, 4/2017
DOI: 10.3290/j.ohpd.a38737, PubMed-ID: 28831461Seiten: 391-397, Sprache: EnglischBassetti, Mario A. / Bassetti, Renzo G. / Sculean, Anton / Salvi, Giovanni E. / Bornstein, Michael M. / Ramseier, Christoph A.Purpose: To evaluate the awareness of cigarette smoking as a risk factor for chronic periodontitis in patients either undergoing active periodontal treatment (APT) or enrolled in supportive periodontal therapy (SPT).
Materials and Methods: Comprehensive tobacco use history was collected with a questionnaire in 50 patients before and after APT (test) and in 50 patients (control) enrolled in SPT at the School of Dental Medicine, University of Bern. Carbon monoxide (CO) exhalation levels were measured in both APT and SPT patients.
Results: In the test group, 94% (n = 47) completed the study. Before APT, 48% of these (n = 24) knew about the association between smoking and periodontal disease, while 42% (n = 21) assumed a possible association and 10% (n = 5) did not. Following APT, 53% (n = 25) knew about the association, while 34% (n = 17) still assumed a possible association and 10% (n = 5) did not. In the control group, 60% (n = 30) of SPT patients knew about the association of smoking with periodontal disease, while 30% (n = 15) assumed an association and 10% (n = 5) were not aware of any association. In both APT and SPT patients, neither between-group nor baseline to follow-up differences were detected (p > 0.05).
Conclusions: Brief interventions for tobacco cessation during APT or SPT failed to increase periodontal patients' awareness of smoking as a risk factor for chronic periodontitis. In order to both increase awareness and motivation to quit tobacco use, more counseling than conventional brief interventions may be needed.
Key words: chronic periodontitis, exhaled carbon monoxide, patient education, risk factor, smoking, smoking cessation
Schlagwörter: chronic periodontitis, exhaled carbon monoxide, patient education, risk factor, smoking, smoking cessation
International Journal of Periodontics & Restorative Dentistry, 4/2017
DOI: 10.11607/prd.2844, PubMed-ID: 28609492Seiten: 481-489, Sprache: EnglischBender, Philip / Salvi, Giovanni E. / Buser, Daniel / Sculean, Anton / Bornstein, Michael M.The purpose of this retrospective radiographic study was to evaluate and correlate the dimensions and morphology of peri-implant bone defects as determined via cone beam computed tomography (CBCT) scans with regard to the selected treatment approach. Vertical and horizontal peri-implant bone defects (mesial, distal, mesio-oral, mesiobuccal, disto-oral, distobuccal, oral, and buccal) in peri-implantitis cases were measured. Three-dimensional data and defect morphology were correlated to the treatment approach chosen (explantation versus implant retention). A total of 19 patients and 28 implants met the inclusion criteria, resulting in a sample size of 224 sites and a total of 896 measurements. The mean percent bone loss did not correlate to the type of treatment chosen (P = .1286). In contrast, when only the maximum vertical values per implant were selected, maximum percent bone loss exhibited a significant correlation to the type of treatment chosen (P = .0021). The effect of the defect morphology on the treatment strategy chosen did not show a statistically significant correlation (P = .4685). Based on the data presented, the maximum bone loss around the implant seems to be a critical factor in deciding whether or not an implant should be explanted. The use of CBCT for treatment planning in cases of peri-implantitis can offer valuable additional information but should be considered only after initial clinical examination and two-dimensional imaging.
Implantologie, 1/2017
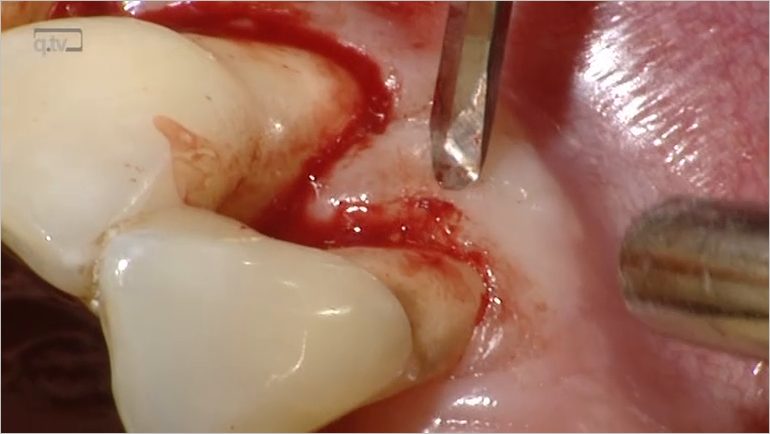
Seiten: 61-75, Sprache: DeutschBassetti, Mario A. / Salvi, Giovanni E. / Sculean, Anton / Bassetti, Renzo G.Ein FallberichtEine bestehende chronische Parodontitis stellt ein erhöhtes Risiko für einen Implantatmisserfolg dar. Nur eine umfassende Therapie der Parodontitis, mit dem Ziel einer taschenfreien Dentition (keine parodontale Resttasche mehr > 5 mm) vor der Implantatinsertion, kann dieses Risiko wesentlich reduzieren. Aber auch nach erfolgreichem Abschluss einer aktiven Parodontitistherapie ist die strikte und engmaschige supportive Parodontaltherapie (SPT) von entscheidender Bedeutung, um biologische Langzeitkomplikationen einer Implantattherapie zu vermeiden. Das Ziel dieses Fallberichts ist, ein mögliches klinisches Vorgehen aufzuzeigen, wie eine konsequente parodontale Vorbehandlung und anschließende Langzeitbetreuung optimale Voraussetzungen für eine aufwendige implantatgetragene Rekonstruktion schaffen.
Schlagwörter: Parodontitisvorgeschichte, nichtchirurgische Parodontaltherapie, Lappenoperation, Sinusbodenelevation, Vollzirkonarbeiten, Zahnimplantate
Parodontologie, 4/2016
Seiten: 413-423, Sprache: DeutschPirracchio, Luca / Sculean, Anton / Salvi, Giovanni E.Molaren mit Furkationsbeteiligung sind die am schwierigsten zu behandelnden Zähne und stellen den Behandler vor eine Herausforderung. Die komplizierte Anatomie erschwert den Zugang sowohl für die häusliche als auch für die professionelle Zahnreinigung, was Furkationen zu permanenten Nischen für bakterielle Ablagerungen macht. Um diese bakteriellen Nischen zu eliminieren und somit weiteren Attachmentverlust zu verhindern, bietet sich die resektive Furkationstherapie an. Die häufigsten Komplikationen resezierter Molaren stellen Wurzelfrakturen und endodontische Misserfolge dar. Die Langzeitüberlebensrate resezierter Molaren ist mit derjenigen von Implantaten in Molarenposition vergleichbar und bietet daher eine realistische Behandlungsalternative.
Schlagwörter: Furkation, resektive Furkationstherapie, Biofilm, Wurzelfraktur
Quintessence International, 4/2016
DOI: 10.3290/j.qi.a35132, PubMed-ID: 26574612Seiten: 293-296, Sprache: EnglischSchwarz, Frank / Becker, Kathrin / Bastendorf, Klaus-Dieter / Cardaropoli, Daniele / Chatfield, Christina / Dunn, Ian / Fletcher, Paul / Einwag, Johannes / Louropoulou, Anna / Mombelli, Andrea / Ower, Philip / Pavlovic, Pedja / Sahrmann, Philipp / Salvi, Giovanni E. / Schmage, Petra / Takeuchi, Yasuko / Van Der Weijden, Fridus / Renvert, StefanAir polishing was introduced as an alternative approach for the supra- and submucosal biofilm management at dental implants. An international expert meeting involving competent clinicians and researchers took place during the EUROPERIO 8 conference in London, UK, on 4 June 2015. Prior to this meeting a comprehensive systematic review dealing with the efficacy of air polishing in the treatment of peri-implant mucositis and peri-implantitis was prepared and served as a basis for the group discussions. This paper summarizes the consensus statements and practical recommendations on the clinical application of air polishing for the management of peri-implant mucositis and peri-implantitis.
Schlagwörter: air polishing, peri-implantitis, peri-implant mucositis, therapy
Quintessence International, 6/2015
DOI: 10.3290/j.qi.a33688, PubMed-ID: 25699298Seiten: 499-510, Sprache: EnglischBassetti, Mario / Kaufmann, Regula / Salvi, Giovanni E. / Sculean, Anton / Bassetti, RenzoBackground: Scientific data and clinical observations appear to indicate that an adequate width of attached mucosa may facilitate oral hygiene procedures thus preventing peri-implant inflammation and tissue breakdown (eg, biologic complications). Consequently, in order to avoid biologic complications and improve long-term prognosis, soft tissue conditions should be carefully evaluated when implant therapy is planned. At present the necessity and time-point for soft tissue grafting (eg, prior to or during implant placement or after healing) is still controversially discussed while clinical recommendations are vague.
Objectives: To provide a review of the literature on the role of attached mucosa to maintain periimplant health, and to propose a decision tree which may help the clinician to select the appropriate surgical technique for increasing the width of attached mucosa.
Results: The available data indicate that ideally, soft tissue conditions should be optimized by various grafting procedures either before or during implant placement or as part of stage-two surgery. In cases, where, despite insufficient peri-implant soft tissue condition (ie, lack of attached mucosa or movements caused by buccal frena), implants have been uncovered and/or loaded, or in cases where biologic complications are already present (eg, mucositis, peri-implantitis), the treatment appears to be more difficult and less predictable.
Conclusion: Soft tissue grafting may be important to prevent peri-implant tissue breakdown and should be considered when dental implants are placed. The presented decision tree may help the clinician to select the appropriate grafting technique.
Schlagwörter: peri-implant keratinized attached mucosa, peri-implantitis, soft tissue recession
Quintessence International, 1/2015
DOI: 10.3290/j.qi.a32817, PubMed-ID: 25262675Seiten: 31-41, Sprache: EnglischHägi, Tobias T. / Hofmänner, Petra / Eick, Sigrun / Donnet, Marcel / Salvi, Giovanni E. / Sculean, Anton / Ramseier, Christoph A.Objectives: To characterize the physical characteristics of a new low abrasive erythritol powder (EPAP) and to evaluate its influence on the clinical and microbiologic parameters over a period of 6 months in patients undergoing supportive periodontal therapy (SPT).
Method and Materials: Prior to the clinical application, the particle size and abrasion level of EPAP were compared to glycine air-polishing powder (GPAP) ex vivo. Subsequently, 40 chronic periodontitis patients previously enrolled in SPT were randomly assigned into two groups for the treatment with subgingival EPAP or repeated scaling and root planing (SRP). At baseline (BL), bleeding on probing positive (BOP+) sites with probing pocket depth (PPD) of ≥ 4 mm but no detectable calculus were defined as study sites. During SPT, these sites were either treated by EPAP or SRP at BL, 3, and 6 months (3M, 6M). When indicated, additional SRP was provided. Plaque Index, BOP, PPD, clinical attachment level (CAL), and subgingival plaque were evaluated at BL and 6M.
Results: EPAP yielded lower abrasiveness and smaller particle sizes when compared to GPAP. In 38 patients completing the study, EPAP and SRP resulted in significant reductions of BOP% (EPAP, 40.45%; SRP, 42.53%), PPD (EPAP, -0.67; SRP, -0.68), and increase of CAL (EPAP, 0.48; SRP, 0.61) while at 6M no statistically significant between-group differences were observed (P > .05). Microbiologic evaluation revealed minor shifts in the composition of the subgingival biofilm without influence on periodontopathogenic bacteria.
Conclusion: The subgingival use of EPAP by means of an air-polishing device may be considered safe and may lead to comparable clinical and microbiologic outcomes to those obtained with SRP. Clinical Relevance: The subgingival use of EPAP appears to represent a promising modality for the removal of subgingival biofilm during SPT.
Schlagwörter: air polishing, bleeding on probing, erythritol, hard tissue loss, supportive periodontal therapy