Quintessence International, 4/2024
DOI: 10.3290/j.qi.b5104947, PubMed-ID: 38502155Seiten: 314-326, Sprache: EnglischNagy, Pal / Nemeth, Florina / Ghanaati, Shahram / Heselich, Anja / Windisch, PeterObjectives: This case series aimed to assess the efficacy of a novel horizontal ridge augmentation modality using histology. Combinations of “sticky bone” and tenting screws without autologous bone were used as augmentative materials.
Method and materials: Five individuals presenting healed, atrophic, partially edentulous sites that required horizontal bone augmentation before implant placement were enrolled. Patients underwent the same augmentation type and 5 months of postoperative reentry procedures. The first surgery served as implant site development, whereas the biopsy and corresponding implant placement were performed during reentry. The bone was qualitatively analyzed using histology and histomorphometry and quantitatively evaluated using CBCT.
Results: Four individuals healed uneventfully. Early wound dehiscence occurred in one case. Histology showed favorable bone substitute incorporation into the newly formed bone and intimate contact between de novo bone and graft material in most cases. Histomorphometry revealed an average of 48 ± 28% newly formed bone, 19 ± 13% graft material, and 33 ± 26% soft tissue components. The CBCT-based mean alveolar ridge horizontal increase was 3.9 ± 0.6 mm at 5 months postoperatively.
Conclusions: The described augmentation method appears suitable for implant site development resulting in favorable bone quality according to histology. However, clinicians must accommodate 1 to 2 mm of resorption in augmentative material width at the buccal aspect.
Schlagwörter: autologous platelet concentrates, histology, histomorphometry, horizontal augmentation, sticky bone, tenting screw
International Journal of Periodontics & Restorative Dentistry, 2/2024
DOI: 10.11607/prd.6458, PubMed-ID: 37722007Seiten: 213-218, Sprache: EnglischShahbazi, Arvin / Windisch, Péter / Tubbs, R. Shane / Decater, Tess / Urbán, István A. / Baksa, Gábor / Iwanaga, JoeGuided bone regeneration (GBR) requires a tension-free flap without damaging the collateral circulation in order to secure better surgical outcomes. Topographic knowledge regarding the neurovascular bundles in the posterior aspect of the mandible can prevent complications during lingual flap design. The lingual branch (LB) of the inferior alveolar or maxillary arteries is not sufficiently illustrated or described in the literature. Nevertheless, it has an intimate relationship with the lingual nerve (LN) during ridge augmentation and implant-related posterior mandible surgery. Therefore, this study aimed to clarify the morphology and topography of the LB related to GBR surgeries. In the present human cadaveric study, the LB was analyzed in 12 hemimandibles using latex injection and corrosion casting. Two types of LB were identified based on their origin and course. The LB was found in a common connective tissue sheath close to the LN. The LB assembled several anastomoses on the posterior lingual aspect of the mandible and retromolar area. The LB acted as an anatomical landmark in identifying LN at the posterior lingual aspect of the mandible.
Quintessence International, 5/2023
DOI: 10.3290/j.qi.b3857209, PubMed-ID: 36723496Seiten: 358-370, Sprache: EnglischNagy, Pal / Porzse, Virag / Nemeth, Florina / Windisch, Peter / Palkovics, DanielObjectives: The aim of this report was to present the effectiveness of a novel augmented corticotomy performed before orthodontic treatments in the prevention of buccal alveolar dehiscence and gingival recession.
Method and materials: Four periodontally healthy individuals presenting crowding and thin bone morphotype in the mandibular anterior area were treated with a double-layer tunnel flap, piezotomy, and hard and soft-tissue augmentation. Patients were divided into two groups according to the utilized graft material. The exclusive use of demineralized bovine bone minerals (group 2) was compared to the use of autologous concentrated growth factor-enriched bone graft matrix, “sticky bone” (group 1). CBCT measurements were performed before and 6 months after surgery. Orthodontic treatment was initialized 1 week after surgery.
Results: Postoperative wound healing was uneventful, and tooth alignments were successful in all cases. Postoperative buccal hard tissue dimensions were favorable in both groups, with no occurring bone dehiscence or gingival recession. The seemingly better results of group 2, in terms of quantitative hard tissue changes, did not have any clinical significance according to the objective to be achieved. In contrast, qualitative radiographic analysis showed a more homogenous tissue formation around teeth in group 1.
Conclusion: It can be concluded that the presented preorthodontic treatment approach seems to be successful in preventing alveolar dehiscence and gingival recession around buccally inclined mandibular anterior teeth.
Schlagwörter: alveolar bone regeneration, alveolar dehiscence, growth factors, minimally invasive flap, periodontally accelerated osteogenic orthodontics, sticky bone
Quintessence International, 6/2022
DOI: 10.3290/j.qi.b2793209, PubMed-ID: 35274512Seiten: 492-501, Sprache: EnglischPalkovics, Daniel / Molnar, Balint / Pinter, Csaba / Gera, Istvan / Windisch, PeterObjective: The aim of the current article was to present a radiographic method to determine the surface area of newly formed periodontal attachment, as well as to analyze volumetric and morphologic changes after regenerative periodontal treatment.
Method and materials: In this retrospective study, 11 singular intrabony periodontal defects were selected for minimally invasive surgical treatment and 3D evaluation. 3D virtual models were acquired by the segmentation of pre- and postoperative CBCT scans. This study determined the surface area of baseline periodontal attachment (RSA-A) and defect-involved root surface (RSA-D) on the preoperative 3D models, and the surface area of new periodontal attachment (RSA-NA) on the postoperative models. Finally, cumulative change of periodontal attachment (∆RSA-A) was calculated and Boolean subtraction was applied on pre- and postoperative 3D models to demonstrate postoperative 3D hard tissue alterations.
Results: The average RSA-A was 84.39 ± 33.27 mm2, while the average RSA-D was 24.26 ± 11.94 mm2. The average surface area of RSA-NA after regenerative periodontal surgery was 17.68 ± 10.56 mm2. Additionally, ∆RSA-A was determined to assess the overall effects of ridge alterations on periodontal attachment, averaging 15.53 ± 12.47 mm2, which was found to be statistically significant (P = .00149). Lastly, the volumetric hard tissue gain was found to be 33.56 ± 19.35 mm3, whereas hard tissue resorption of 26.31 ± 38.39 mm3 occurred.
Conclusion: The proposed 3D radiographic method provides a detailed understanding of new periodontal attachment formation and hard tissue alterations following regenerative surgical treatment of intrabony periodontal defects.
Schlagwörter: 3D evaluation, CBCT segmentation, minimally invasive periodontal surgery, new periodontal attachment, regenerative periodontal surgery, root surface area
International Journal of Computerized Dentistry, 3/2021
SciencePubMed-ID: 34553889Seiten: 241-251, Sprache: Englisch, DeutschPalkovics, Daniel / Pinter, Csaba / Bartha, Ferenc / Molnar, Balint / Windisch, PeterZiel: Ziel dieses Artikels ist es, eine neuartige Methode der DVT-Subtraktionsanalyse von 3-D-Veränderungen des Kamms nach Alveolarkammerhaltung vorzustellen, die mit räumlicher Bildregistrierung und halbautomatischer Segmentierung arbeitet. Studienhypothese war, dass bei Verwendung unseres neuen Ansatzes eine bessere 3-D-Visualisierung und bessere volumetrische und lineare Bewertung der Kammrekonstruktion nach Alveolarkammerhaltungstechnik möglich ist als mit den bereits existierenden Verfahren.
Material und Methode: Zehn Stellen bei 10 teilbezahnten Patienten wurden zur Alveolarkammerhaltung mit einer gesteuerten Knochenregeneration (GBR) in Tunneltechnik behandelt. Mittels räumlicher Bildregistrierung und einer halbautomatischen Segmentierungsmethode wurden digitale 3-D-Modelle der prä- und postoperativen DVT-Daten für eine Subtraktionsanalyse generiert. Primäre Ergebnisvariable der Studie war die Volumendifferenz zwischen dem prä- und dem postoperativen DVT-Scan. Als sekundäre Ergebnisvariablen wurden horizontale und vertikale lineare Messungen an der mesialen und distalen Seite der Alveole sowie in deren Mitte ausgewertet.
Ergebnisse: Die Veränderung des Hartgewebevolumens betrug im Durchschnitt 0,34 ± 0,99 cm3. Die mittlere Veränderung der vertikalen Knochenhöhe lag bei 5,97 ± 3,18 mm an der mesialen Seite, 6,40 ± 3,03 mm an der distalen Seite und 7,01 ± 3,02 mm in der Mitte der Extraktionsstelle. Die horizontale Knochenbreite veränderte sich im Durchschnitt an der mesialen Seite um 6,19 ± 0,68 mm, an der distalen Seite um 6,32 ± 1,52 mm und in der Mitte der Extraktionsstelle um 6,90 ± 1,48 mm.
Schlussfolgerung: Die digitale Rekonstruktion von DVT-Daten nach dem hier vorgestellten Ansatz ermöglicht ein besseres Verständnis der Heilungsmechanismen nach Alveolarkammerhaltung. Neben der direkten Wirkung auf die Heilung der Extraktionsalveole lässt sich auch der indirekte positive Effekt für die angrenzenden Zähne visualisieren.
Schlagwörter: 3-D-Modellerstellung, Alveolarkammerhaltung, radiologische Bildrekonstruktion, Segmentierung, Volumetrie
International Journal of Periodontics & Restorative Dentistry, 3/2020
Seiten: 321-330, Sprache: EnglischNagy, Pal / Molnar, Balint / Nemes, Balint / Schupbach, Peter / Windisch, PeterThe aim of this case series was the histologic evaluation of guided tissue regeneration utilizing deproteinized bovine bone mineral (DBBM) when regenerative surgery was combined with (test) or without (control) early orthodontic tooth movement. Core biopsy samples were harvested from previously defected sites after 9 months. The histologic section showed integration of DBBM particles in newly formed bone in the apical and middle thirds of the defect, while in the coronal part, graft materials were mainly embedded in connective tissues in the control patient. DBBM particles showed partial resorption with more de novo bone formation in test samples.
Parodontologie, 1/2020
Seiten: 89-92, Sprache: DeutschWindisch, PéterInternational Journal of Periodontics & Restorative Dentistry, 6/2019
DOI: 10.11607/prd.4106, PubMed-ID: 31613946Seiten: 845-852, Sprache: EnglischMolnár, Bálint / Deutsch, Tibor / Marton, Rita / Orbán, Kristóf / Martin, Anna / Windisch, PeterThe objective of this study was to compare the novel extraction-site development (XSD) technique with spontaneous healing. Advanced alveolar defects (extraction defect sounding, classes 3 and 4) at 33 single-rooted teeth were treated by XSD (test), and 21 extraction sites of single-rooted teeth were left for spontaneous healing (control). In pre- and postoperative cone beam computed tomography (CBCT) data sets, orovestibular and vertical socket dimensions were assessed, as were socket areas. XSD resulted in complication-free healing with significantly higher radiographic bone fill compared to spontaneous healing. Application of the XSD approach may reduce the need for augmentative procedures during implant placement.
Quintessence International, 7/2017
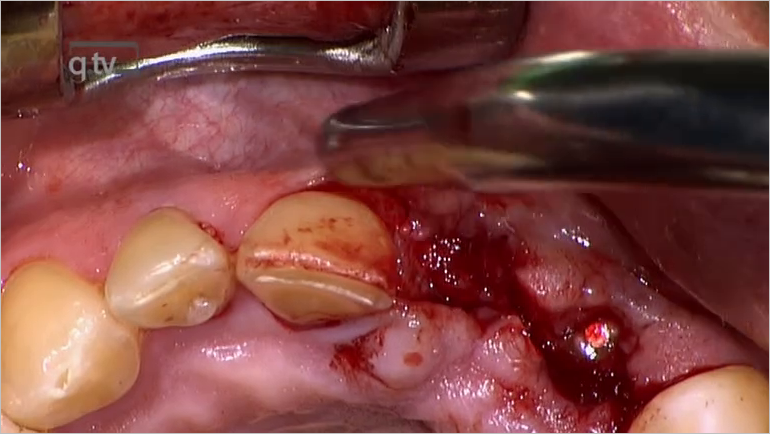
DOI: 10.3290/j.qi.a38354, PubMed-ID: 28555201Seiten: 535-547, Sprache: EnglischWindisch, Peter / Martin, Anna / Shahbazi, Arvin / Molnar, BalintObjective: To introduce a novel split-thickness flap design without periosteal and vertical releasing incisions for horizontovertical ridge augmentation.
Method and Materials: Three patients with generalized chronic periodontitis presented posterior partial edentulism with class C alveolar defects according to the horizontal, vertical, and combination (HVC) classification. In all three cases, implant placement and simultaneous horizontovertical ridge augmentation utilizing a novel split-thickness flap design was performed. Hard tissue reconstruction was followed by additional soft tissue grafting at membrane removal if optimal peri-implant soft tissue stability could not be ensured. Following abutment connection, fixed implant-retained partial dentures were fabricated.
Results: The healing procedure after surgeries was uneventful in all cases, without any serious local or systemic adverse events. After 9 months of healing, complete pocket resolution without gingival recession was observed at neighboring teeth with periodontal attachment loss. A comparison of the mean bone to implant/screw contact at first surgery and at membrane removal demonstrated a mean crestal bone regeneration of 3.08 ± 1.25 mm. At 12 months after prosthetic loading, signs of positive bone remodeling and crestal bone maintenance were shown on intraoral radiographs in all cases. Radiographic results showed maintained alveolar crest contours during 60 months of follow-up in all three cases.
Conclusion: The clinical and radiographic observations of the three presented cases demonstrate that the guided bone regeneration technique utilizing titanium membranes in combination with autologous and xenogeneic grafting materials applied with the presented split-thickness flap resulted in predictable three-dimensional reconstruction of hard tissues.
Parodontologie, 2/2017
Seiten: 169-171, Sprache: DeutschWindisch, Peter